Bed sores, also called pressure sores or decubitus ulcers, are an unpleasant and uncomfortable condition. They commonly appear on bony areas of the body, such as the hips, tailbone, elbows, heels, and ankles, and can result in tissue damage and even tissue death due to reduced blood flow to the affected area. People who are unable to move around frequently, such as those who are bedridden or use a wheelchair, are at a higher risk of developing bed sores. In this article, we will explore the facts about bed sores that everyone should know.
Causes Sof Bed Sores
Bedsores are the result of a combination of four primary factors: pressure, friction, shear, and constant moisture on the skin. These factors can lead to compression of the skin and underlying tissues, which can cause the death of tissue. Let’s explore the primary causes of bed sores.
Pressure
Bed sores can occur when there is prolonged pressure on the skin, even if the pressure is relatively low. This constant pressure can reduce blood flow to the affected area, leading to tissue damage and breakdown. As a result of breakdown, ulcers start to form on the skin, especially if the pressure is not relieved and the area is not properly cared for. In some cases, high pressure over a shorter period of time can also cause bed sores to form.
Friction And Shear
Friction and shear forces have a significant impact on the formation of bed sores. These forces happen when the skin is dragged against a surface, resulting in the blood vessels being stretched and torn. Consequently, The reduced blood flow may damage the cells. The rubbing of the skin against still surfaces may cause the skin’s top layer to come off, leading to swelling and breaking the barrier against infections.
Moisture
Constant presence of moisture can contribute to the development of bed sores by increasing the skin’s susceptibility to damage from pressure and other external factors. When the skin is constantly wet, it becomes more vulnerable to damage, and in some cases, too much moisture alone can lead to skin ulceration.
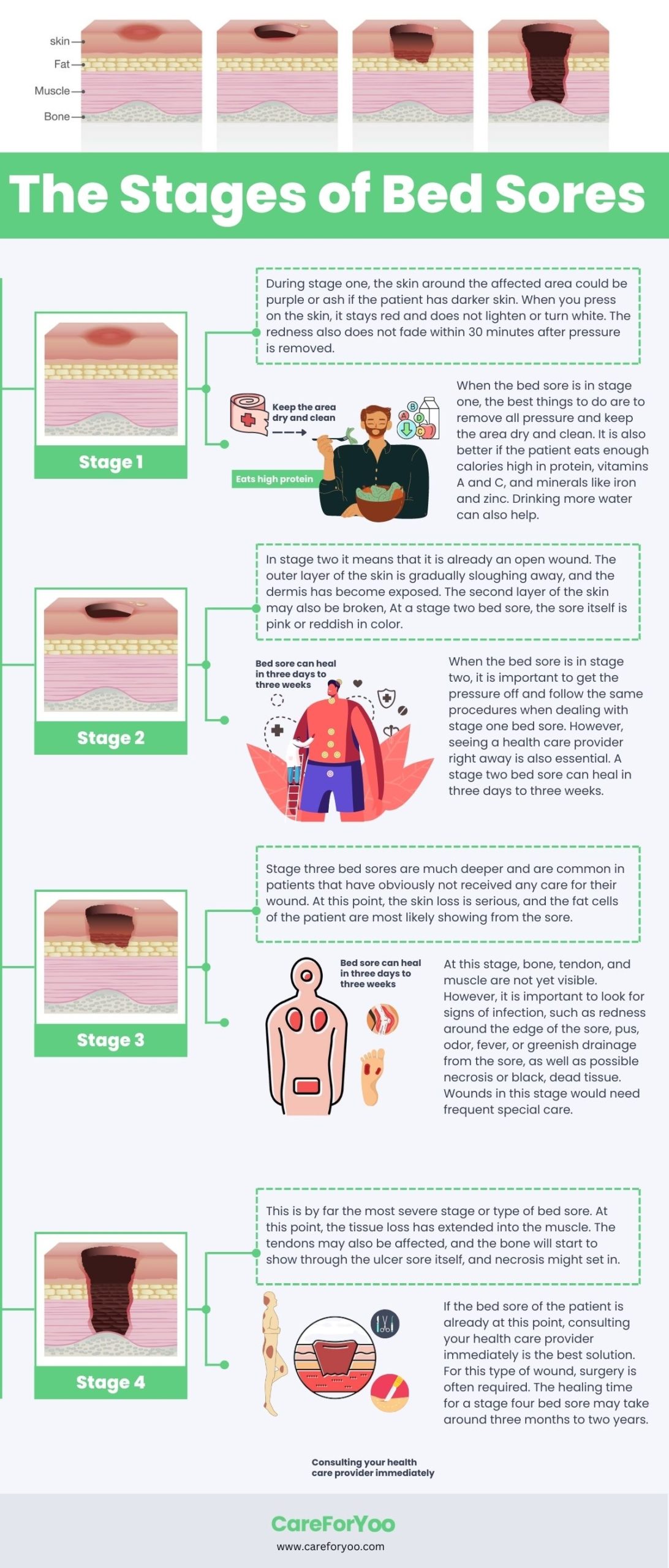
Stages of Bed Sores
When you visit the doctor for bed sore treatment, they might want to know which stage your bed sore is in. So, let’s go over the different stages of bed sores and what symptoms to look out for:
Stage 1
In stage 1 bed sores, the skin is the least damaged. They may feel a little sore or itchy, but they don’t usually cause any other symptoms. If you see a red area on your skin that doesn’t lighten after pressing on it for some time, this means the area isn’t getting enough blood flow. It can be hard to tell if this is happening in darker skin.
Stage 2
In stage 2 of bed sores, the sore digs deeper below the skin’s surface, causing more damage. The affected skin is broken and may resemble a blister filled with pus or clear fluid. The area is usually swollen, red, and warm to the touch. Additionally, the sore can be quite painful.
Stage 3
In stage 3 of bed sores, the ulcer has progressed through the first two layers of skin and is now in the layer of fat underneath. This can cause symptoms like a deep wound that smells bad, signs of infection, and black tissue surrounding the sore.
Stage 4
The fourth and final stage of bed sores is the most severe. It can get very deep and the skin can turn black. There may be signs of infection, such as red edges, pus, and odor. Sometimes tendons, muscles, and even bones can be seen in stage 4 bedsores.
Complications Of Bed Sores
Complications can occur in stage 4, and some of the infections that can lead to life-threatening conditions are listed below:
Cellulitis
Cellulitis affects the skin and underlying tissues, causing symptoms such as redness, swelling, and warmth in the affected area. People with nerve damage may not feel any pain, making it even more important to regularly check for signs of this infection.
Bone And Joint Infection
Bed sore can penetrate into the bones and joints, leading to conditions such as septic arthritis and osteomyelitis. These infections can damage the cartilage and tissue, causing reduced function of the limbs and joints.
Sepsis
When bedsores are left untreated, they can become infected, leading to sepsis. Sepsis is a potentially life-threatening condition that occurs when bacteria from an open sore enters the bloodstream and can cause organ failure if left untreated.
Prevention Of Bed Sores
Bed sores can be a painful and debilitating condition, but fortunately, there are steps you can take to prevent them:
Keep Changing Positions To Relieve Pressure
To prevent bed sores, you need to move around a lot and relieve pressure as often as possible. This will help keep the skin healthy and prevent damage. Your healthcare team will create a repositioning timetable that takes your individual needs into account. You may need to adjust your sitting and lying positions frequently, at least every two hours.
Avoid Dehydration And Take Proper Nutrition
Bed sores can be prevented and treated by proper nutrition and hydration. Studies suggest that increased intake of certain nutrients such as energy, protein, zinc, vitamins A, C, and E, as well as specific amino acids like arginine and glutamine, can promote wound healing.
Adequate hydration is also essential for maintaining and repairing skin integrity. It is recommended to consume at least 1.6 to 2 liters of fluids per day. Maintaining a healthy weight can also reduce the risk of developing bed sores.
Use Specialized Support Surfaces
Bed sores can be prevented and treated by using special surfaces that help reduce pressure on the wound. These surfaces can be classified into three different types based on their power and effectiveness.
- Using foam, gel, or air to help reduce pressure on your skin can help if you are at low risk of developing bed sores or if you have Stage 1 bed sores.
- Some mattresses use a pump to switch between different levels of pressure, which can help reduce the pressure on the skin. These mattresses are designed for patients who are at moderate risk of developing bed sores, or for patients who have already developed Stage 2 bed sores.
- Air-fluidized beds help distribute pressure evenly across the surface, which makes them ideal for people who are at high risk of developing bed sores or for patients who have already developed Stage 3 or Stage 4 bedsores.
Treatment Of Bed Sores
Bed sores can be treated several ways depending upon the severity. Here are the treatments commonly used:
Wound Care
The severity of bed sores determines the treatment required for wound care, which involves using a gentle cleanser to clean the area and drying it. Open sores require the use of a saltwater solution or water each time the dressing is changed, and a bandage is recommended to keep the wound moist, prevent infection, and keep the surrounding skin dry. There are various types of bandages available, such as films, gauzes, gels, foams, treated coverings, and a combination of these may be necessary.
Medications
To manage bed sores, specialized dressings such as alginate and hydrocolloid can be used to speed up the healing process. Other types of dressing such as foams, films, gels, and antimicrobial dressings can also be used. Creams and ointments are generally not recommended, but barrier creams may be necessary to protect irritated skin.
Antibiotics can be prescribed to treat infected ulcers or more severe infections like blood poisoning, bacterial infections in the tissue under the skin, and bone infections. A balanced diet with enough nutrients can further speed up the healing process.
Surgery
In severe cases of pressure ulcers, surgery may be necessary to prevent life-threatening infections and promote healing. During surgery, the damaged tissue is removed to allow healthy tissue to heal more quickly, but this creates a larger wound.
After surgery, bedrest is required for several months to avoid any pressure on the wound, which could delay healing or worsen the injury. Surgery offers several benefits, such as a shorter recovery time, improved quality of life, increased independence, and lower healthcare costs.
However, surgery also carries potential risks, including wound recurrence, improper healing, infections, tissue death, and bleeding. The patient must balance the benefits against the possible risks when deciding on surgery.
Psychological Impact And Emotional Support
The development of bed sores not only causes physical discomfort and pain, but also affects the psychological well-being of patients as well as people around them. Research has shown that patients with bedsores are more likely to suffer from pessimism and depression, impacting their nutrition, healing ability, and overall quality of life.
Furthermore, the presence of bed sores can lead to emotional and psychological trauma, including feelings of shame and embarrassment. Patients may also develop a fear of being a burden on others and experience social isolation, impacting their relationships.
Therefore, emotional support is important to address these psychological effects and improve the patient’s overall well-being. Caregivers and healthcare providers must provide proper emotional support to help patients cope with the distressing social and psychological effects of bed sores.
Conclusion
Bed sores are a painful and potentially life-threatening condition that can be caused by prolonged pressure, friction and shear, and moisture. Prevention and early intervention is the key to reducing the risk of developing bed sores and achieving better outcomes. This includes changing positions regularly, proper nutrition and hydration, and the use of specialized support surfaces. It’s important to be aware of the different stages of bed sores and to seek medical attention promptly if you notice any symptoms. By taking these preventative measures, we can reduce the chances of of bedsores development and improve the quality of life for those who are at risk.